By Dr. Tarik Hadid
Wayne State University
Human papillomavirus (HPV) is a small DS-DNA virus, and humans are the only known hosts. There are around 200 subtypes of the virus that can be classified into cutaneous vs. mucosal. 40 different HPV subtypes are sexually transmitted, HPV infects the basal cell of the different cell layers that form the skin or mucosa, and it is a local infection, meaning that the virus doesn’t circulate in the blood. Only a few subtypes of HPV are high-risk and directly linked to different types of epithelial carcinomas. HPV-related oropharyngeal squamous cell carcinoma (OPSCC) became the most common HPV-related cancer in the US, bypassing cervical cancers in 2015.
The incidences of HPV-related OPSCC continue to rise, and the most common HPV subtype that causes OPSCC is subtype-16. HPV integrates the E6 and E7 oncogenes into the host cell, which leads to the inactivation of several tumor suppressor genes, including silencing the retinoblastoma gene (Rb) and p53 gene. HPV-mediated OPSCC is associated with improved progression-free survival (PFS) and overall survival (OS) compared to HPV-negative OPSCC. This difference in survival is likely due to differences in tumor biology and sensitivity to treatment. This prompted the American Joint Commission on Cancer to recognize HPV-mediated OPSCC as a separate entity in its 8th edition.
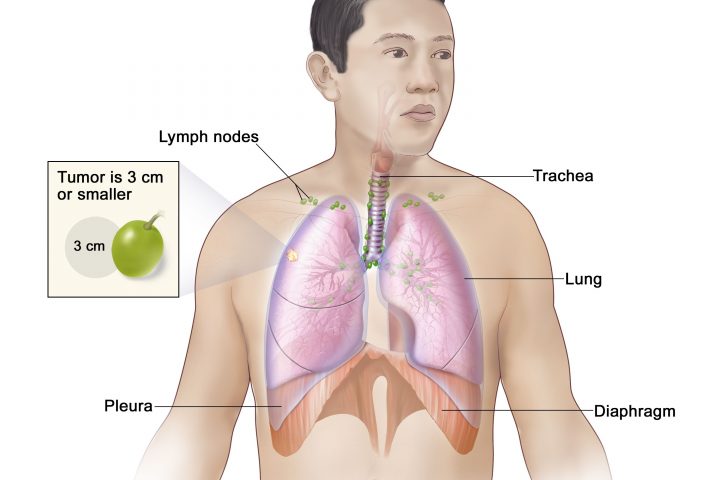
Treatment of localized and locally advanced OPSCC is challenging and remarkably toxic. The use of radiation therapy (RT) together with chemotherapy is highly effective in irradicating malignancy but with multiple short and long-term treatment-related sequelae and functional abnormalities. While this is predominantly due to the use of high doses of RT (≈70 Gy), the addition of chemotherapy also contributes to this toxicity and augments the toxic effect of RT. Therefore, there has been growing interest in treatment de-escalation, particularly in low-risk HPV-mediated OPSCC patients, which are defined as being T1 or T2 disease, with or without low-volume cervical lymph nodes metastases, but no more than N1 disease, and having ≤10 pack-year history of smoking. This definition was established based on a retrospective review of multiple studies including the RTOG 0129 trial, that identified this group of patients with an OS of 93%, in which de-escalation can be considered [1].
Several methods of treatment de-escalation have been attempted to reduce treatment-related toxicity. The initial attempt to reduce toxicity used intensity-modulated RT (IMRT) rather than conventional RT. Using this technique has been shown to reduce several toxic side effects such as xerostomia, weight loss, speech deficits, trismus, and dysphagia [2] and is now the standard treatment modality in most cancer centers. Reducing the dose of RT is associated with lower toxicity. Several phase II studies have examined reducing the RT dose. For example, the NRG-HN002 trial evaluated reduced-dose RT at 60 Gy in patients with low-risk OPSCC given with chemotherapy and reported a 2-year PFS of 90.5% [3]. Another phase II trial evaluated 60 Gy of IMRT concurrently with chemotherapy and reported 2-year PFS and OS of 86%, and 95%, respectively. The authors of this study concluded that with these favorable outcomes, neither neoadjuvant chemotherapy nor routine surgery is needed to obtain favorable results [4]. There is an ongoing phase II trial (NCT03323463) evaluating major RT dose reduction to 30 Gy given concurrently with cisplatin in patients with HPV-related OPSCC T1-2N1-2bM0 OPSCC and comparing it to standard chemoradiation [5]. To date, reducing RT dose in HPV-related OPSCC remains an experimental approach and should not yet be performed outside the clinical trial setting.
Changing the type of systemic therapy has also been attempted to reduce toxicity. Cetuximab has been proposed as a treatment de-escalation in HPV-mediated OPSCC. Three phase III trials (RTOG 1016, De-ESCALaTE HPV, and TROG 12.01) compared cetuximab to cisplatin in low-risk HPV-mediated OPSCC. They all showed statistically significant detriment in PFS with the former two trials showing detriment in OS as well for patients treated with cetuximab without significant reduction in toxicity [6-8]. Data regarding integrating immunotherapy in the treatment of OPSCC is in its infancy. OPTIMA 2 evaluated nivolumab with nab-paclitaxel and carboplatin followed by risk and response-guided de-intensification for locally advanced HPV-mediated OPSCC. Those with a low-risk disease with ≥ 50% reduction in tumor size were treated with transoral robotic surgery (TORS) or 50 Gy of RT. Low-risk patients with <50% reduction in tumor size were treated with chemoradiotherapy at 45–50 Gy. The 2-year PFS and OS for the full cohort were 90.4% and 93.3%, respectively. Although the concept of substituting concurrent cisplatin chemotherapy with immunotherapy is intriguing, it is still in the experimental phase [9].
Using surgery to reduce the RT dose or eliminate the need for RT and chemotherapy has been proposed for treatment de-escalation. Retrospective studies initially suggested better outcomes with transoral robotic surgery (TORS) compared to standard chemoradiation [10]. Prospectively, ORATOR, a phase II trial randomized 68 HPV-unselected T1-2, N0-2 (≤4 cm) OPSCC to 70 Gy of RT with chemotherapy (if N1-2) or TORS and neck dissection (with or without adjuvant chemoradiotherapy). Results showed that 100% of patients in the RT group could have an oral diet without restrictions compared with 84% of patients in the TORS group (P=0.055). Overall, patients treated with RT had superior swallowing-related quality of life (QOL) scores at 1 year, which persisted but decreased over time. One patient in the TORS arm died from catastrophic bleeding [11, 12]. This was followed by ORATOR2, a phase II trial that evaluated the use of primary RT to TORS approach as a treatment de-escalation modality for HPV-related OPSCC. After recruiting 61 patients, the study was halted due to excessive toxic effects in the TORS arm, which included 3 deaths, 2 of them were treatment-related and one from myocardial infarction. One patient developed local recurrence in the TORS arm as well. Grade 2 to 5 toxic effects occurred in 20 patients (67%) in the RT arm and 22 (71%) in the TORS. Swallowing related QOL scores at 1 year were similar between the two arms [13].
In summary, de-escalation techniques in low-risk HPV-mediated OPSCC are evolving. While the outcome of using TORS and cetuximab have been disappointing, reducing definitive RT dose appears to be feasible and is being actively investigated in clinical trials. Incorporating immunotherapy in treatment de-escalation techniques is also promising and is being further researched to reduce toxicity while maintaining excellent survival outcomes.
References
1. Ang, K.K., et al., Human Papillomavirus and Survival of Patients with Oropharyngeal Cancer. New England Journal of Medicine, 2010. 363(1): p. 24-35.
2. Bird, T., et al., Outcomes of intensity-modulated radiotherapy as primary treatment for oropharyngeal squamous cell carcinoma – a European singleinstitution analysis. Clin Otolaryngol, 2017. 42(1): p. 115-122.
3. Yom, S.S., et al., Reduced-Dose Radiation Therapy for HPV-Associated Oropharyngeal Carcinoma (NRG Oncology HN002). J Clin Oncol, 2021. 39(9): p. 956-965.
4. Chera, B.S., et al., Phase II Trial of De-Intensified Chemoradiotherapy for Human Papillomavirus-Associated Oropharyngeal Squamous Cell Carcinoma. J Clin Oncol, 2019. 37(29): p. 2661-2669.
5. Clinicaltrials.gov. Major De-escalation to 30 Gy for Select Human Papillomavirus Associated Oropharyngeal Carcinoma. 2023; Available from: https://clinicaltrials.gov/ct2/show/NCT03323463.
6. Mehanna, H., et al., Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet, 2019. 393(10166): p. 51-60.
7. Rischin, D., et al., Randomized Trial of Radiation Therapy With Weekly Cisplatin or Cetuximab in Low-Risk HPV-Associated Oropharyngeal Cancer (TROG 12.01) – A Trans-Tasman Radiation Oncology Group Study. Int J Radiat Oncol Biol Phys, 2021. 111(4): p. 876-886.
8. Gillison, M.L., et al., Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet, 2019. 393(10166): p. 40-50.
9. Zhou, X. and X. Wang, Radioimmunotherapy in HPV-Associated Head and Neck Squamous Cell Carcinoma. Biomedicines, 2022. 10(8).
10. Nguyen, A.T., et al., Comparison of Survival After Transoral Robotic Surgery vs Nonrobotic Surgery in Patients With Early-Stage Oropharyngeal Squamous Cell Carcinoma. JAMA Oncology, 2020. 6(10): p. 1555-1562.
11. Nichols, A.C., et al., Radiotherapy versus transoral robotic surgery and neck dissection for oropharyngeal squamous cell carcinoma (ORATOR): an open-label, phase 2, randomised trial. Lancet Oncol, 2019. 20(10): p. 1349-1359.
12. Nichols, A.C., et al., Randomized Trial of Radiotherapy Versus Transoral Robotic Surgery for Oropharyngeal Squamous Cell Carcinoma: Long-Term Results of the ORATOR Trial. J Clin Oncol, 2022. 40(8): p. 866-875.
13. Palma, D.A., et al., Assessment of Toxic Effects and Survival in Treatment Deescalation With Radiotherapy vs Transoral Surgery for HPV-Associated Oropharyngeal Squamous Cell Carcinoma: The ORATOR2 Phase 2 Randomized Clinical Trial. JAMA Oncol, 2022. 8(6): p. 1-7.