Leaders in Health Equity Honored by the Binaytara Foundation
Announcing the 2024 Award Recipients for Humanitarianism, Distinguished Faculty, and Volunteer of the Year
Statement from Dr. Binay Shah
The Binaytara Foundation (BTF) is a global cancer non-profit dedicated to improving access to cancer care in the United States and abroad through education and innovative program models that break down barriers and advance best practices in hematology and oncology. The Binaytara Foundation’s major projects include hematology and oncology conferences and the establishment of a cancer hospital in Nepal. Donate here!
The Binaytara Foundation’s annual awards for Humanitarianism, Distinguished Faculty, and Volunteer of the Year will be presented at this year’s gala, to be held on April 27, 2024, from 6:00-8:30 PM, at the Grand Hyatt in Seattle, Washington. The event will include entertainment, live and silent auctions, dining, learning, friendship, and more – all in support of BTF’s mission. Purchase tickets here!
2024 Distinguished Faculty
The Binaytara Foundation’s Distinguished Faculty Award recognizes individuals who have demonstrated long-standing excellence in teaching and improving access to education for healthcare providers.

This year’s Distinguished Faculty Awards go to Dr. George Rodgers and Dr. Ulka Vaishampayan.
Dr. Vaishampayan and Dr. Rodgers have been valued members of the Binaytara Foundation Faculty Community, extensively contributing as distinguished speakers at national conferences. Their insights and presentations consistently receive high acclaim from both colleagues and participants. Thank you, Dr. Vaishampayam and Dr. Rodgers, for your vital role in advancing the Binaytara Foundation’s mission!

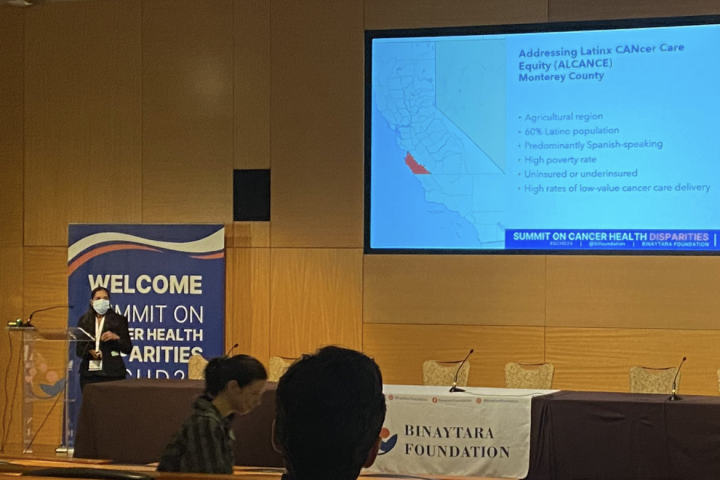
2024 Humanitarian Award
The Binaytara Foundation Humanitarian Award recognizes individuals who demonstrate the foundation’s core values through their volunteer work, community engagement, and dedication to improving access to cancer care.

This year’s award will be presented to Dr. Ana María López, a trailblazer in health equity research, relentlessly advancing diversity, equity, and inclusion in medicine. Her leadership at the Binaytara Foundation’s Summits on Cancer Health Disparities has been pivotal in driving critical conversations and actions to address cancer health disparities. Congratulations, Dr. López, on your impactful work!
2024 Volunteer of the Year
Dr. Anish Shah will be named the Binaytara Foundation’s Volunteer of the Year for 2024. Dr. Anish Shah, originally from Janakpur, Nepal, has played
 an instrumental role in implementing electronic medical records at the Binaytara Foundation Cancer Hospital in Nepal. We deeply appreciate Dr. Shah’s dedication and impactful contributions. Thank you, Dr. Shah!
an instrumental role in implementing electronic medical records at the Binaytara Foundation Cancer Hospital in Nepal. We deeply appreciate Dr. Shah’s dedication and impactful contributions. Thank you, Dr. Shah!