By: Dr. Arya Mariam Roy
Roswell Park Comprehensive Cancer Center
What are immune checkpoint inhibitors?
Immune checkpoint inhibitors are a type of immunotherapy that harnesses the body’s own immune system to prevent the growth of cancer cells. Nowadays, these inhibitors are approved to treat various cancer types including melanoma (a type of skin cancer), kidney cancer, breast cancer, bladder cancer, cervical cancer, colon cancer, head and neck cancer, Hodgkin lymphoma (cancer of the lymph nodes), liver cancer, lung cancer, stomach cancer, and others.
What is the mechanism of action of immune checkpoint inhibitors?
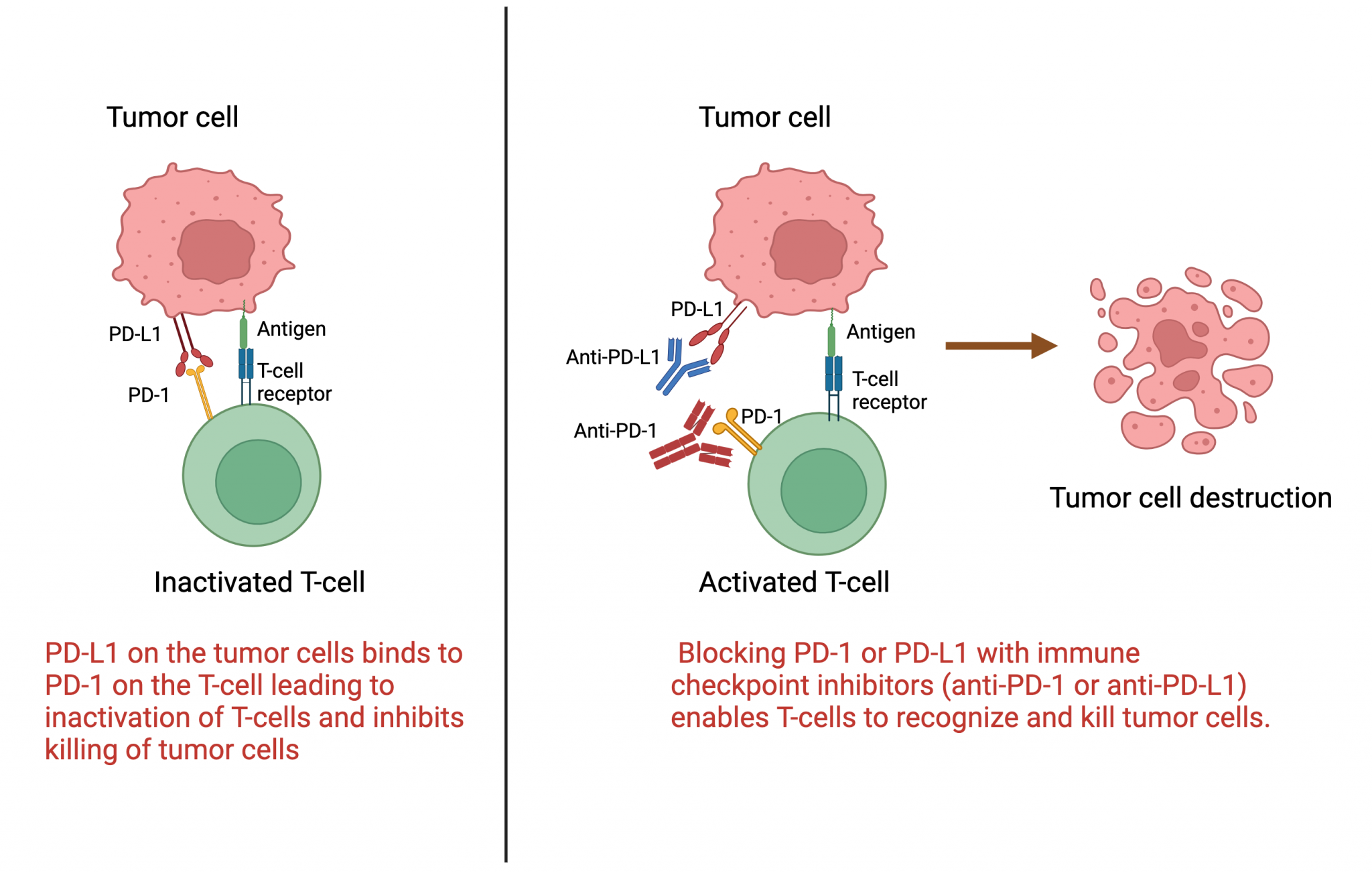
Immune checkpoints are natural regulators of the immune system, designed to prevent an immune response from becoming too aggressive and attacking healthy cells. These checkpoints come into play when proteins on the surface of immune cells, known as T cells, recognize and interact with partner proteins on certain tumor cells. These partner proteins are referred to as immune checkpoint proteins.
Immune checkpoint inhibitors are medication that targets specific proteins in the body’s immune system, such as PD-1 (programmed cell death protein 1) and PD-L1 (programmed death-ligand 1). These proteins act as “brakes” on the immune system, preventing it from attacking healthy cells. However, cancer cells can exploit these brakes by producing high levels of PD-L1, which then binds to PD-1 on the T cells, effectively turning off their ability to attack the cancer.
Immune checkpoint inhibitors work by blocking the interaction between PD-1 and PD-L1. One type of immune checkpoint inhibitor targets a protein called CTLA-4, while others focus on a protein known as PD-1 (anti-PD-1) or its partner protein, PD-L1 (anti-PD-L1). This essentially releases the brakes on the immune system, allowing it to recognize and attack cancer cells more effectively (Figure 1). It is essentially removing the disguise worn by cancer cells, enabling the immune system to identify them as threats and mount a targeted attack.
What are the side effects of immune checkpoint inhibitors?
Immune checkpoint inhibitors have revolutionized cancer treatment, but they can also cause side effects, known as immune-related adverse events (irAEs). These side effects occur because immune checkpoint inhibitors unleash the immune system, which can lead to attacks on healthy tissues as well as cancer cells.
The side effects of immune checkpoint inhibitors can vary widely and may affect almost any organ system in the body. Common side effects include fatigue, skin rashes, diarrhea, and inflammation of the lungs, liver, or thyroid gland. In some cases, rare side effects such as hepatitis (inflammation of the liver), myocarditis (inflammation of the heart muscle, hypophysitis (inflammation of the pituitary gland)) nephritis (inflammation of the kidney) and impaired kidney function can occur.
The mechanism behind these side effects lies in the immune system’s increased activity. When the immune system is activated by checkpoint inhibitors, it can mistakenly attack normal cells in addition to cancer cells. For example, inflammation of the skin (dermatitis) can occur when immune cells target healthy skin cells, leading to rashes or other skin problems. Similarly, inflammation of the intestines can result in diarrhea, while inflammation of the lungs can cause shortness of breath or coughing.
It’s important for patients receiving immune checkpoint inhibitors to be closely monitored for these side effects, as they can sometimes be serious or even life-threatening. Prompt recognition and management of irAEs are essential for ensuring the safe and effective use of these groundbreaking therapies.