LIBRETTO-431: Randomized phase III study of selpercatinib versus chemotherapy and pembrolizumab in RET fusion-positive advanced NSCLC
Author: Dr. Anam Kamal
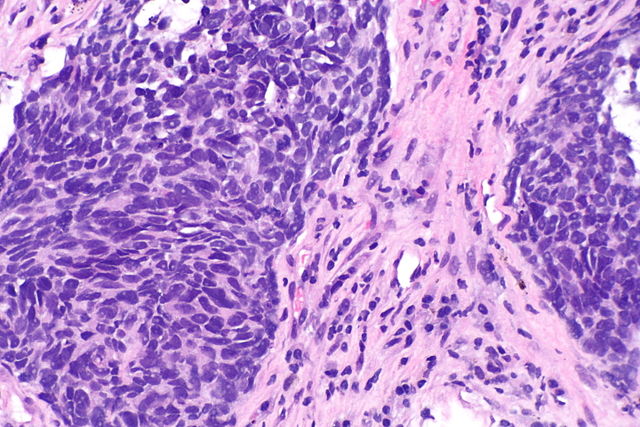
Selpercatinib is a brain penetrant, a highly selective and potent inhibitor of RET signaling that has demonstrated anti-tumor activity in the LIBRETTO-001 phase I/II trial. The study showed a 64% objective response rate (ORR) (95% confidence interval [CI]: 54-73%) in 105 patients with RET fusion-positive (RET +) non-small cell lung cancer (NSCLC) who previously received platinum-based chemotherapy and an 85% ORR (95% CI: 70-94%) in treatment-naïve patients (n=39). Additionally, it demonstrated a median duration of response (DOR) of 18 months (95% CI: 12-not estimable [NE]) in patients who previously received chemotherapy.
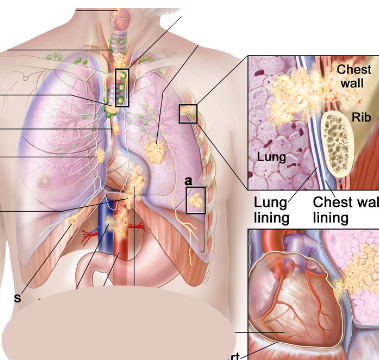
LIBRETTO-431 is a phase 3, randomized, open-label trial that evaluated selpercatinib versus the current standard of care platinum-based chemotherapy (cisplatin or carboplatin) plus pemetrexed with or without pembrolizumab in patients with EGFR/ALK-negative NSCLC. This is the first randomized trial to compare the safety and efficacy of a targeted therapy to a PD-1 inhibitor plus chemotherapy in a biomarker-selected patient population.
A total of 261 patients were enrolled from 23 countries and were randomized to receive selpercatinib 160 mg BID in 3-week cycles (Arm A) or pemetrexed (500 mg/m2 IV) in 3-week cycles plus investigator’s choice of carboplatin (AUC 5) or cisplatin (75 mg/m2 IV) for 4 cycles (Arm B). For patients in Arm B, at the investigator’s discretion, pembrolizumab (200 mg IV) could also be given for up to 35 cycles and patients could receive maintenance pemetrexed +/- pembrolizumab. Crossover to selpercatinib was allowed for Arm B patients who had progression of disease. Stratification factors included geography: East Asian versus non-East Asian, brain metastases: presence versus absence, and intended treatment if randomized to Arm B: +/- pembrolizumab.
The primary endpoint of blinded independent central review (BICR)-assessed PFS was tested first in patients stratified by investigator’s intent to treat with pembrolizumab, if assigned to the control arm, (ITT-pembro) and then in the ITT population. At a median follow up of approximately 19 months, selpercatinib demonstrated superior PFS versus control in the ITT-pembro (HR: 0.465, 95% CI: 0.309, 0.699; p-value <0.001) and ITT populations (HR: 0.482, 95% CI: 0.331, 0.700; p-value <0.001). In the ITT-pembro population, median PFS was 24.8 months (95% Cl: 16.9, NE) with selpercatinib vs 11.2 months (95% CI: 8.8, 16.8) with control. Clinically meaningful improvements in objective response rate (ORR), duration of response (DOR), and intracranial response were also observed with selpercatinib versus control. Time to CNS progression was longer with selpercatinib than control (cause-specific HR 0.61; 95% CI: 0.19, 1.92; p=0.0006). Adverse events observed with selpercatinib and the control arm were generally consistent with those previously reported.
Selpercatinib achieved a statistically significant and clinically meaningful improvement in PFS compared to chemotherapy + pembrolizumab in advanced RET+ NSCLC. These data support comprehensive genomic testing at diagnosis and treatment with first-line selpercatinib in patients with advanced RET+ NSCLC.