Presented by: Dr. Stephen S. Grubbs
As we look at quality through value-based solutions, there are many perspectives to explore and to integrate. Our professional society, the American Society of Clinical Oncology (ASCO) has Certified practices through Patient Centered Cancer Care Standards. This work has been years in the making by building on ASCO’s initial Quality Oncology Practice Initiative (QOPI®) Certification Program, the Oncology Medical Home, and successes in value-based care, such as the Patient Centered Medical Home and the the Community Oncology Medical Home (COME HOME).
This 2012 grant from the Centers for Medicare & Medicaid Services Innovation Center (CMMI) was awarded to Dr. Barbara McAneny to develop and test the COME HOME model. Seven community oncology practices participated and reached more than 2,100 persons with cancer. Project analysis reported improvements in practice workflow, significant reduction in hospital readmissions and emergency room visits, and overall excellent patient satisfaction. Elements of this model were incorporated into the design of the Oncology Care Model (CMMI), a subsequent Oncology Medical Home model (COA and COC), and ASCO Certifications.
The Oncology Medical Home’s (OMH) standards were developed based on the consensus of a multidisciplinary expert panel that included clinicians, health system administrators, and patients/patient advocates and a systematic review of evidence which included comparative peer-reviewed studies, studies of clinical pathways , and a systematic review of survivorship care plans (Figure 1). Once drafted, the standards were approved by COA’s Payment Reform Committee and the ASCO Board of Directors.
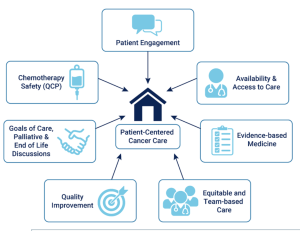

Figure 1
The panelists discussed multiple ways to address our “measurement mess”. The group emphasized the importance of meaningful metrics and to consider quality as an ever-evolving goal. Measure that “matter” focused on access, such as, same day appointments. Ways to get there included moving away from claims data, respecting existing clinical workflows, minimizing burden, developing metrics that have a purpose, and creating partnerships with persons with cancer, their caregivers as “truth-tellers”, and clinical teams. It takes a village.
Developing quality care models is complex and requires addressing payment models and care delivery models. As these pieces are integrated and implemented, the models, the approach, the science will evolve.
This work led to the ASCO Certified Pilot with Certification Standards adopted from Oncology Medical Home Standards. Twelve practices and 2 commercial payers engaged. Certification awards began July 2022 which was followed by pngoing Assessment and Improvement Activities. With equity concerns, ASCO’s Health Equity and Outcomes Committee developed the Equity Quality Improvement Practice (EQuIP) Tool Collaborative to guide assessment of equitable cancer care delivery and to identify and implement quality improvement initiatives. The tool will support sites in meeting the equity standard of ASCO Certified and Enhancing Oncology Model (EOM) consistent with the 4 domains of OMH standards, and the learning collaborative will test the tool to ensure it achieves stated goals and provides a roadmap for continuous quality improvement.
An E-PRO Implementation Collaborative has also been developed and implemented through a PCORI grant which will develop and implement SOPs for PRO collection and to test feasibility of implementation. As we develop value-based models, the patient voice needs to be heard and integrated. The National Coalition for Cancer Survivorship (NCCS) reports annually on a patient and caregiver survey on the cancer care experience.
In the 2023 survey, patients characterized their focus as generally being on eradicating the cancer no matter what, Caregiver focus was generally on maintaining their loved one’s quality of life. The survey reports on the cancer experience and serves to inform what is important to patients and those who love them. Caregivers report grappling with a variety of physical, emotional, and mental health issues of their own. Most Patients remain very satisfied with each stage of their care, and satisfaction has increased this year on several dimensions. Caregivers are significantly less satisfied/more critical with each phase of the care journey. Both caregiver and patient satisfaction is higher among those whose loved-one had received a care plan. The most prevalent symptoms reported were feeling overly tired and having mental health concerns. Women, POC, and younger persons were more likely to experience symptoms. Sixty percent of younger persons with cancer reported mental health issues. The number of persons who were impacted financially decreased slightly nationally; but young, Black, Hispanic, Stage IV, and less educated Patients continue to report more financial hardship. Caregivers also reported higher rates of financial consequences.