Presented by: Eric Collisson, MD, Professor of Medicine, Helen Diller Comprehensive Cancer Center
Covered by: Inas Abuali, MD, FACP

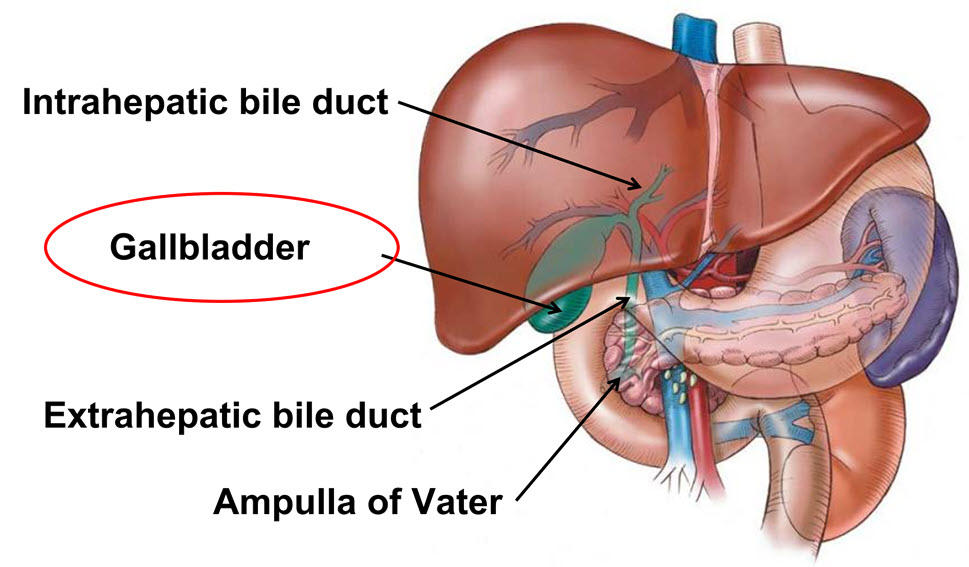
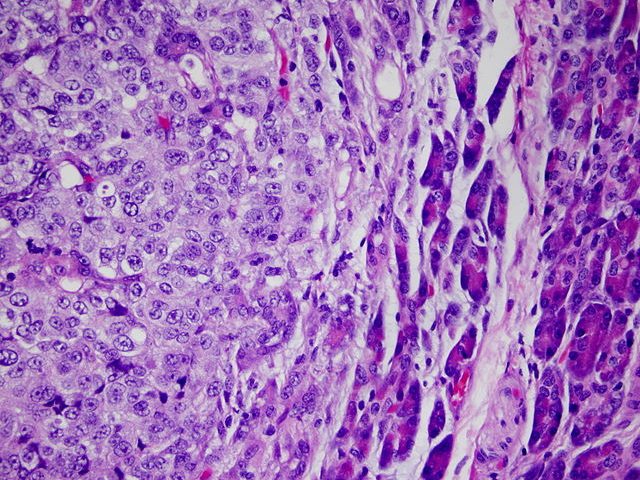
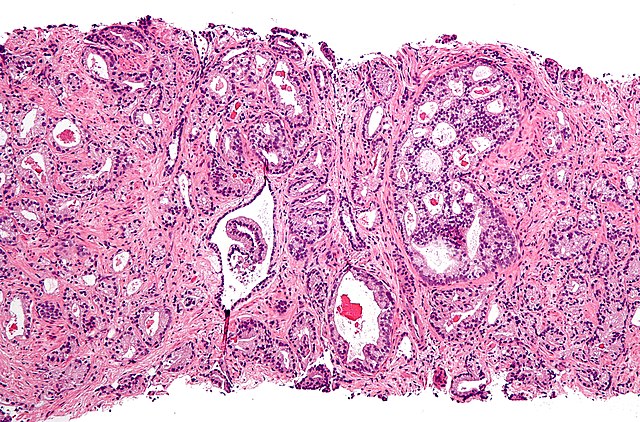
In the first half of this session, Dr. Collisson highlights the anatomic and genomic heterogeneity of biliary tract malignancies, and the efficacy of targeted therapies against mutated oncogenes. Approximately one third of patients with intrahepatic cholangiocarcinoma (ICC) have targetable mutations such as FGFR2 fusions and rearrangements, IDH1 mutations and BRAF V600E mutations.
While detection of FGFR2 fusions can be difficult, they are present in about 10% of patients with ICC. Pemigatinib, an ATP-competitive FGFR inhibitor was approved here in the US in 2020 after demonstrating ORR of 35.5% and a median PFS of 6.9 months. [1] Futibatinib, a covalent inhibitor, received accelerated approval in the US in 2022, with a median PFS of 9 months, and median OS of 21.7 months in the second line setting for FGFR2-rearranged cholangiocarcinoma. [2]
IDH1 mutations occur in approximately 13% of ICC. [3] Ivosidenib, a selective oral inhibitor of mutant IDH1, was approved in 2021 after the ClarIDHy trial demonstrated an improvement in median PFS of 2.7 vs 1.4 months, median OS 10.3 vs 7.5 months and ORR of 2% vs 0% as compared to placebo. [4,5]
Finally, 5-7% of patients with ICC harbor a BRAF V600E mutation and the combination of Dabrafenib with Trametinib can be utilized in this setting with promising response rates.
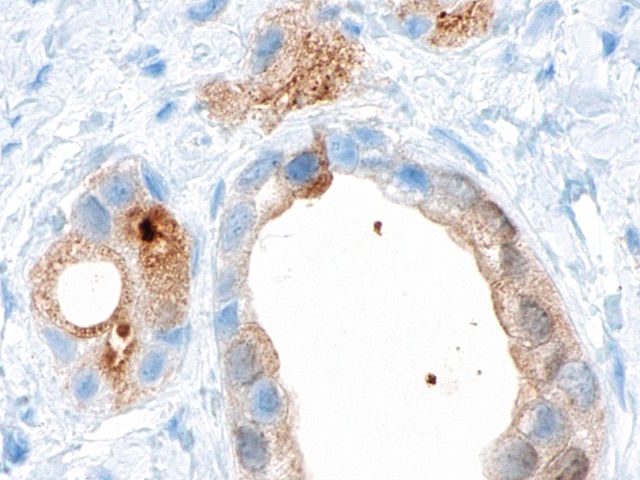
Dr. Collisson then reviewed future directions in the field, with antibodies paving the way to precision enrollment in CAR-T trials. Zolbetuximab is a monoclonal antibody targeting Claudin18.2, a protein expressed in the tight junction of gastric mucosa cells, and its addition to chemotherapy results in improved PFS and OS in gastric malignancies expressing Claudin 18.2.
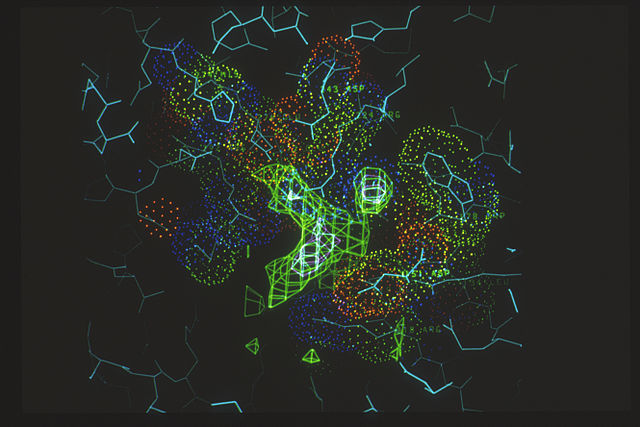
Claudin 18.2 CAR shows early promise in gastric/GEJ malignancies, with ORR of 57.1% and 6-month OS of 81.2% [7] On-target and off-tumor toxicity is a major limitation to the implementation of engineered T cells targeting solid tumors, since almost all potential CAR T cell targets are also expressed on healthy tissue. Therefore, new cellular designs which build circuits for cell-cell recognition and signal integration are necessary to allow for customized sense/response programs. [8] These efforts will eventually move from bench to bedside and revolutionize our current care paradigm.
- Abou-Alfa et al. Lancet Oncol 2020;21:671-84
- Goyal et al NEJM 2023
- Boscoe et al J Gastrointest Oncol 20(4) 2019
- Abou-Alfa et al. Lancet Oncol 21(6) 2020
- Zhu et al. JAMA Oncol 2021;7(11)
- Subbiah Nature Medicine 2023
- Qi et al., May 2022 (Nature Med)
- Morsut et al. Cell 2016